In health, those in safeguarding lead roles find themselves with legislation, statutory guidance and the weight of national scandals highlighting how important leadership is in their role.
Safeguarding professionals are limited to the existing leadership and management approaches that don’t take into account:
- complex organisations without dedicated teams
- safeguarding’s position and structure as typically adjacent to operational hierarchies
- safeguarding roles undertaken on top of substantive posts
- the wider challenges of inter-agency, multi-agency, inter-professional or multi-professional working
Professionals may have well tested leadership and management tools, but the clear need for improvement would suggest they are not the right tools for the job.
The Challenge
In health, statutory guidance offers no position on leadership and management expectations for the role. Safeguarding training in health is built on the Intercollegiate Documents and existing safeguarding leadership and management courses currently only draw on generic theory. The Intercollegiate Documents describe ‘Named’ and ‘Designated’ practitioners as requiring the ability to provide 'expert', 'strategic and professional leadership', but fail to provide guidance on to how to lead without hierarchical power, even if practitioners hold what French and Raven (1959) describe as ‘expert power’.
We have to do better
Leadership in safeguarding means working with others and numerous national scandals show how inadequate leadership potentially harms patients. Older leadership theories popular in health such as ‘Distributed’ and ‘Situational Leadership’ do not always translate well to safeguarding as they rely on power and there is nothing out there that truly captures leading when you’re not in charge. If we expect safeguarding practitioners to be leaders, or leaders to recognise their accountability and responsibility for safeguarding, then they deserve training and the supporting theory that’s fit for purpose.
Health can be proud of how it uses research to inform practice but we have a blind spot for safeguarding, this must be addressed for our colleagues and for those we support.
For a research project as part of the MSc Child Protection and Adults Safeguarding at Buckinghamshire New University, I captured the experience of Safeguarding Leads in health for whom hierarchical authority and positional power is not always available. Building on the experiences shared, the findings facilitated the development of a ‘Reflective Relational model for Leadership and Management’.
The experiences
Three major themes were identified through the study, best summarised as:
- power
- relationships
- the training or support required.
Leads with positional authority spoke about preferring not to use it, instead using the strength of relationships as a preferred source of power. Equally, those without positional authority are limited to using relationships or 'borrowing' power to be effective.
The different sources of power identified by leads can be aligned with the definitions provided by French and Raven (1959) and Hersey et al (1979), leading to a concise reflection of the sources of power in safeguarding:
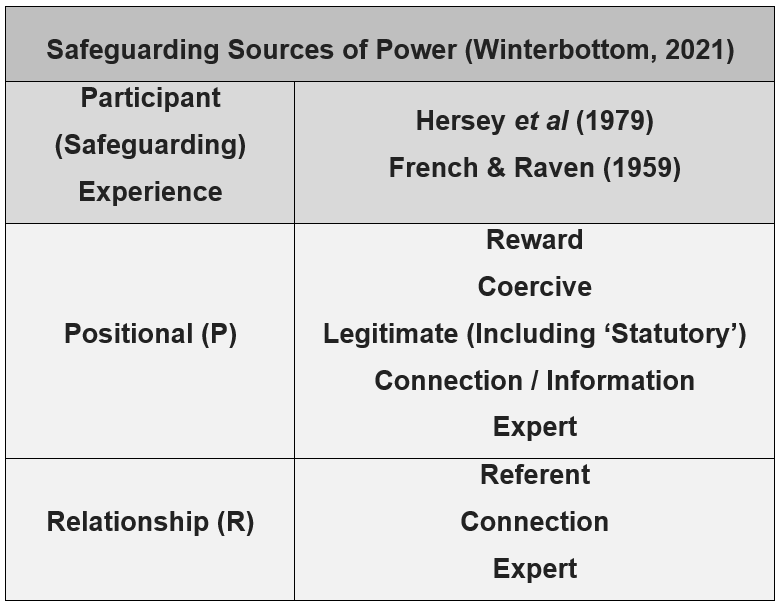
Safeguarding Sources of Power (Winterbottom, 2021)
Does training help?
Participants clearly reflected that leadership and management training doesn’t effectively support safeguarding roles, also that safeguarding training rooted in the intercollegiate documents does not translate into leadership skills. Participants with leadership and management training reflected this challenge, with or without positional authority in their substantive role (the only transferable approach from training discussed was ‘reflective leadership’).
The Solution?
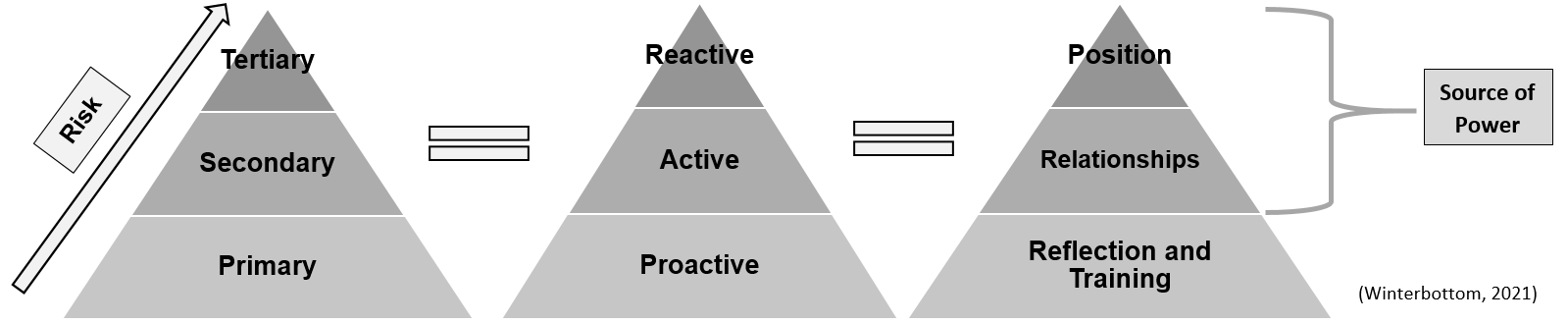
The research project employed a constructivist grounded theory approach, which supported the development of model that captures the inter-play between three main themes where each aspect is dependent on the other. To this effect, training is positioned in the model alongside reflection as an ongoing primary intervention and proactive foundation of practice, supporting relationships, professional identity, recognition of hierarchy, responsibility and accountability which influence the requirement for secondary/active or tertiary/reactive responses.
A recognisable model to build upon is the ‘intervention pyramid’, familiar from its use in public health approaches where risk informs the level of response and primary/proactive interventions are an ongoing foundation. Reflection and training are positioned as a proactive approach, relationships as the preferred active response, then the use of positional power as a last resort.
The research identified Schön’s (1983) reflective model as well suited for inclusion to ensure continuous reflection, something all Leads highlighted the importance of. This is captured in a detailed breakdown of the model, making clearer reference to the experiences shared:
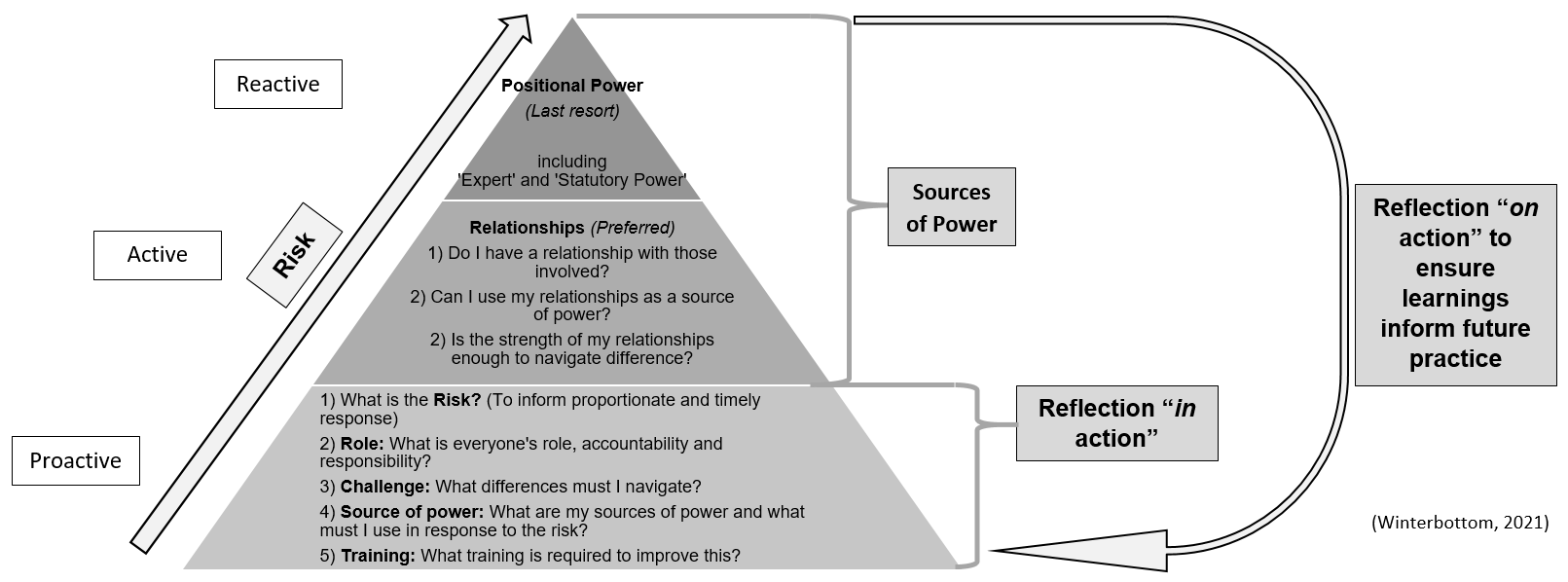
Similarities to Situational Leadership Theory (Hersey et al, 1979) are evident in that the lead must assess the situation and adapt their approach accordingly. However instead of requiring an understanding of a colleague’s motivation and needs (with the assumption of holding the authority to respond accordingly), the Lead is expected to continually reflect on the risk and challenges of the task itself, adapting to use the power available to them.
Simplifying the model allows for interpretation and adaption by individual leaders:
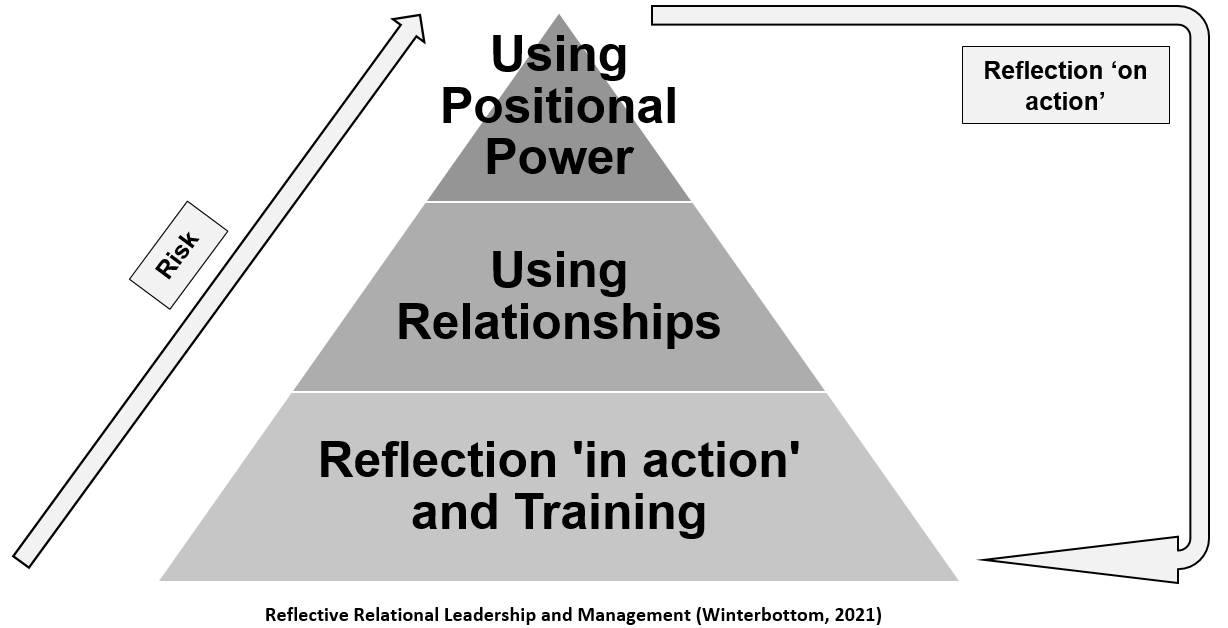
The ‘Reflective Relational’ approach does not require hierarchical authority. The model supports relationships as the primary source of power and does not mandate that safeguarding leads have ‘expert’ power as, despite an assumption by others, the overwhelming reflection regarding training was that it was not as informative as practical experience, something not all leaders or managers will have in the early stages of their careers.
I hope that this new model resonates with safeguarding practitioners across health and potentially leaders and managers across the wider systems. Whilst developed for safeguarding, it could easily be adapted for other areas where the challenge of leading when you’re not in charge is present, or simply for leaders and managers who are committed to a kinder, more compassionate and reflective style that commits to achieving more with sugar than salt.
A video explaining the model is available online.
Questions for Practice
In addition to welcoming any feedback on this blog, questions and challenge about the model, practitioners can ask themselves:
- How they lead and manage, through relationships or other power sources?
- How they build reflection into their work?
- If this model could work for them?
- How the model could apply to roles across the structures in their organisation?

